TITANIUM AS A BIOMEDICAL MATERIAL FOR IMPLANTS
TITANIUM AS A BIOMEDICAL MATERIAL FOR IMPLANTS
Abstract
Titanium are alloy are considered as the most
promising and the most attractive material in the biomedical application. As
titanium has been very long favored for the biomedical application.
However, for permanent implant applications the alloy has a possible toxic
effect resulting from released vanadium and aluminium. For this reason,
vanadium- and aluminium free alloys have been introduced for implant
applications.
Introduction
As material used in the
wide range of the application and must be exhibit and the properties. The main
important of the used in the part of materials used for fabricating implants is
biocompatibility, followed by corrosion resistance. The main metallic
biomaterials are stainless steels, cobalt alloy, and titanium and titanium
alloys. Stainless steel was the first metallic biomaterial used successfully as
an implant. In 1932, the cobalt-based alloy named Vitallium was developed for
medical applications. Titanium is the newest metallic biomaterial. In both
medical and dental fields, titanium and its alloys have demonstrated success as
biomedical devices
The titanium is used in
the biomedical industry due to the excellent mechanical properties and the good
biocompatibility as the titanium as some of the steel, its density is only half
as the steel. The titanium is uses broadly use in the number of field,
including aerospace, power generation,
automotive, dental and medical industries. The first metal alloy developed
specifically for human use was the “vanadium steel” but it was no longer used
in implants because its corrosion resistance is inadequate in vivo. Later in
the 1950s, 18-8sMo with very low carbon content (known as 316L) stainless steel
was introduced and is actually widely used for implant fabrication. This alloy
has a very good resistance to chloride solutions and poor sensitoion. Since the 1960s, titanium has become a
popular metallic biomaterial because of its properties for many biomechanical
applications including dentistry. Although there is an increasing trend for
metal-free restorations in the dental profession,
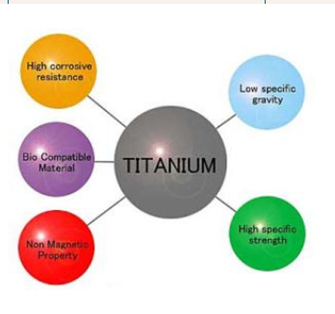
Material properties of
Titanium
Titanium is often used either as the pure metal, or in an
alloyed form in aerospace applications, and in medical and dental work. It is
commonly alloyed with other metals such as Vanadium and Aluminum . It forms
then light-weight but at the same time strong alloys for the fabrication of
oral implants or the frameworks for FDPs.
According to the American Society of Testing Materials, cpTi is available in four different grades that is based on the incorporation of small amounts of oxygen, nitrogen, hydrogen, iron and carbon during purification procedures, where each grade has different physical and mechanical properties. Grades I and II are the most commonly used cpTi types for the production of metal-ceramic FDPs. In oral implants and implant-supported FDPs, cpTi and its alloys exhibit remarkable advantages due to their excellent biocompatibility, corrosion resistance, high strength, and low modulus of elasticity .Yet, the recent trends in making dental biomaterials more biomimetic from both biomechanical and biological perspectives, also applied for cpTi. Principally, the stress transfer between a metal framework and the dental tissues or bone is not homogeneous since stiffness of the metal framework or implants and such tissues are different. This phenomenon is described as “stress shielding”. In order to avoid devitalization of the tooth and atrophy in the bone under chewing function , high Young’s modulus of cpTi compared to those of the tooth and the bone structures, is not desirable. Young’s moduli of the most widely used SUS316L stainless steel and Co-Cr for orthopaedic implant devices, are approximately 180 GPa and 210 GPa, respectively whereas Young’s moduli of cpTi and its alloys are generally lower than those of stainless steels and Co-Cr alloys.
Titanium and biocompatibility
Because the focus of
biomaterials has shifted more towards, tissue engineering, complex medical
application and biotechnology, it has become necessary to better define and
evaluate the specific interaction between biomaterials and tissues .Biocompatibility
refer to the ability of the biomaterial to perform the desire function with the
respect to medical therapy
Beside
the artificial bones, joints replacement and the dental implants, titanium
based alloy also used in the cardiovascular implants
Titanium medical specification
Bone and Joint Replacement
About one million patients worldwide are
treated annually for total replacement of arthritic hips and knee joints. The
prostheses come in many shapes and sizes. Hip joints normally have a metallic
femoral stem and head which locates into an ultrahigh molecular weight low
friction polyethylene socket, both secured in position with polymethyl
methacrylate bone cement. Some designs, including cementless joints, use
roughened bioactive surfaces (including hydroxyapatite) to stimulate
osseointegration, limit resorption and thus increase the implant lifetime for
younger recipients. Internal and external bone-fracture fixation provides a
further major application for titanium as spinal
fusion devices, pins, bone-plates, screws, intramedullary nails, and external
fixators
Maxillofacial and
Craniofacial Treatments
Surgery to repair facial damage using
the patients own tissue cannot always obtain the desired results. Artificial
parts may be required to restore the ability to speak or eat as well as for
cosmetic appearance, to replace facial features lost through damage or disease titanium
implants meeting all the requirements of biocompatibility and strength have
made possible unprecedented advances in surgery, for the successful treatment
of patients with large defects and hitherto highly problematic conditions.
Titanium is regularly used for pacemaker
cases and defibrillators, as the carrier structure for replacement heart
valves, and for intra-vascular stents.
External Prostheses
Titanium is suitable for both temporary
and long term external fixations and devices as well as for orthotic callipers
and artificial limbs, both of which use titanium extensively for its light
weight, toughness and corrosion resistance.
Surgical Instruments
A wide range of
surgical instruments are made in titanium. The metal’s lightness is a positive
aid to reducing any fatigue of the surgeon. Instruments are frequently anodised
to provide a non reflecting surface, essential in microsurgical operations, for
example in eye surgery. Titanium instruments withstand repeat sterilisation
without compromise to edge or surface quality, corrosion resistance or
strength. Titanium is non magnetic, and there is therefore no threat of damage
to small and sensitive implanted electronic devices.
Titanium for dental implant
In this era the
chemical pure titanium is the dominant and very useful material for the dental
implant there has been major change occur in the change in restorative dental
practice worldwide has been possible through the use of titanium implants. A
titanium ‘root’ is introduced into the jaw bone with time subsequently allowed
for osseointegration. The superstructure of the tooth is then built onto the
implant to give an effective replacement.
Surface modification of dental implant
There has been huge research
has been proven on surface modification of micro and nanorough for titanium and
titanium implants. If the relatively impact structure replaced with the
nanostructure surface and coating numerous possibilities of the structure lead
to the significant improvement in the field industry tissue.
The mechanical methods
most widely used in obtaining rough and smooth ti and ti based alloy surface
and its fabrication nanophase surface layer and subtraction and attrition
process.
Conclusion
As the titanium and its
alloy are considered as most promising material among the wide range of the
application. Due to his unique combination of the high strength to weight ratio
, melting temperature and the corrosion resistance . The principal alloys in
practical use are commercially pure titanium. The mechanical properties of the
latter are better, but the slight concern over the biological effects of the
very minor amounts of aluminium and vanadium that they release means that cpTi
is the more widely used of the two. Despite these concerns, there is a large
amount of experimental evidence to show that both alloys have good bioactivity
and the ability to osseointegrate. Additionally, there are few, if any,
accounts of adverse effects arising from release of aluminium and/or vanadium
from dental implants, probably because amounts released are so low. The use of
the titanium is in the very wide area such as it is use in the mediacl field in
bone and joint replacement,
cardiovascular process, surgical instrument. And the main use of the
titanium is in the dental application and it is useful in many fields. For this
reason, the two well-established alloys of titanium continue to be used for the
overwhelming majority of implants used in dentistry, and this use seems likely
to continue for the foreseeable future.




Comments
Post a Comment